
Providing children access to necessary health services in schools increases accessibility to health care and health equity. These school based services for Medicaid eligible children are run at the federal government level, however each state has its own nuances of how to document, validate, and bill for Medicaid services to get reimbursed to receive funding back from the government.
Districts often encounter barriers that block maximizing and using Medicaid reimbursement to support school-based health services. The process for reimbursement is complicated and varies by state. However, done correctly and by working together, states and school districts can receive sustainable funding from CMS if they can systematize and optimize their efforts. Medicaid has revenue earmarked annually for schools in each state, and your district is allowed to bill Medicaid for services but claiming for reimbursement is not automatic. The responsibility falls entirely on your district to claim every cost, and in a compliant manner. That doesn’t mean you need to figure this out on your own!
At Relay we recognize the need for states to have up-to-date information regarding the coverage, eligibility, and billing of Medicaid. Therefore, we recently created individual state resource pages to help school districts understand the Medicaid program in each of their geographical locations—by providing information to answer common questions we receive from districts:
View State PagesYour ultimate guide to find what to bill for in Medicaid will be found in your state Medicaid manual. However, you can check the Relay map, which provides a bulleted, summarized list of services that are covered by your state-specific Medicaid program. For example, you will see that most states cover services like speech and OT services, but only certain states allow you to bill for transportation to and from services.

Each individualized page from our map walks you through the billing eligibility in the states. For example, does your state have an infant and toddler program, or does eligibility only begin at school age? Mostly, all services are pursuant to IEP and end when the child reaches around 21 years of age—but each state has its own definition of Medicaid eligibility. What is yours?
Usually, the LEAs are the billing providers, but some states also have their charter schools, ESA, or ISD as billing providers. Within this section, you will also find out if rendering providers need to be enrolled in Medicaid to participate. Rendering providers, are those that are delivering the services themselves. Some states require that not only the district be enrolled in Medicaid but their staff who are providing billing services be enrolled as well under separate identification numbers.
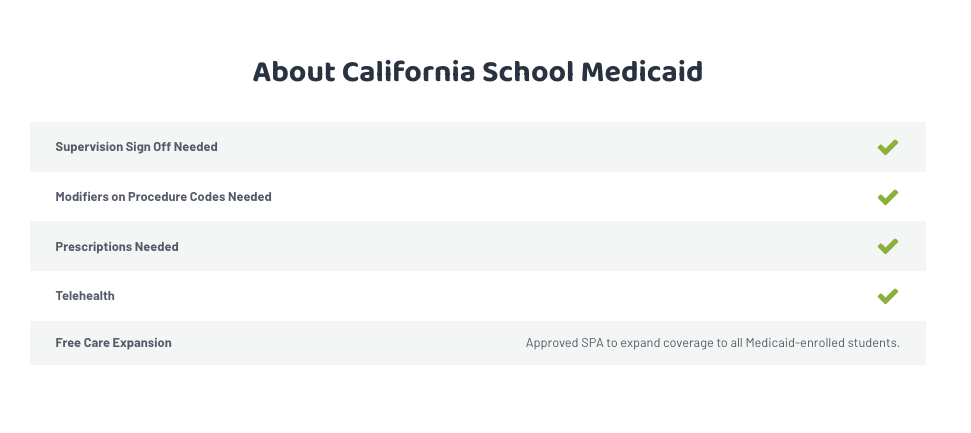
In addition, each state page has a snapshot of quick facts about your state’s Medicaid program, including information on Free Care participation, Telehealth coverage, and more.
Our state pages offer a bridge to the best information you can find in school based Medicaid—with links at the bottom to take your knowledge to the next step, including state-specific and national resources, like Healthy Schools Campaign that all provide an in-depth analysis of billing requirements.
You will also see an opportunity to get in touch with the Relay team—ready to help you understand the process, check on your Medicaid state plan, or just review your current Medicaid program—regardless of you Medicaid billing vendor.
Get in Touch